Introduction
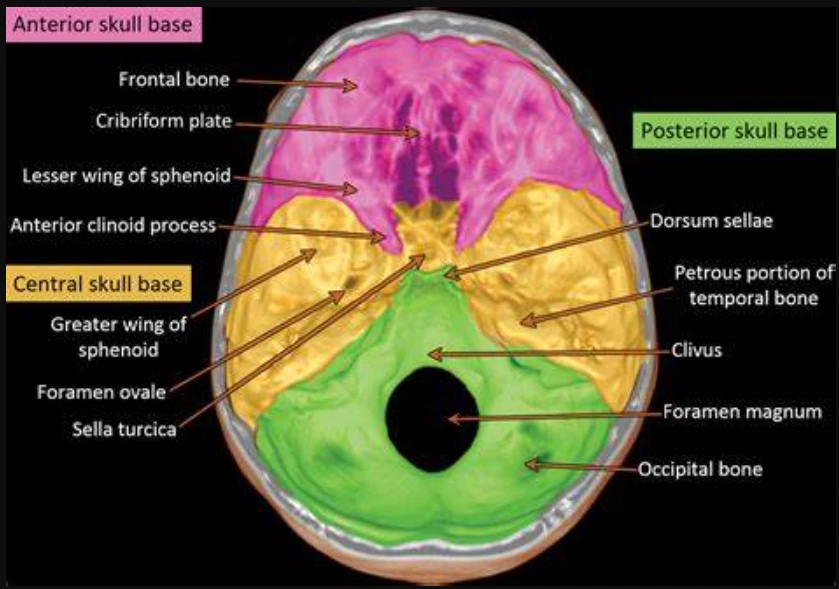
Central skull base osteomyelitis (CSBO) is a rare but serious condition characterized by
infection and inflammation of the bone at the base of the skull, often involving areas like the clivus, sphenoid bone, and adjacent regions. Unlike traditional skull base osteomyelitis, which typically arises as a complication of external otitis (ear infections),
CSBO is more commonly associated with sinus infections, immunocompromised states, or
spread from deep-seated infections. Its insidious nature and potential involvement of critical neurovascular structures make early diagnosis and treatment essential to avoid life-threatening complications.
Causes and Risk Factors
Infectious Agents:
- Pseudomonas aeruginosa: A common pathogen in traditional osteomyelitis involving the ear but less common in CSBO.
- Aspergillus and Mucormycosis: Fungal infections, especially in immunocompromised patients (e.g., those with diabetes or undergoing chemotherapy).
- Staphylococcus aureus: Sometimes implicated, particularly in post-surgical or trauma-related infections.
Risk Factors:
- Diabetes mellitus: The most common predisposing condition.
- Immunocompromised States: Including HIV, post-transplant patients, or those on long-term corticosteroids.
- Chronic Sinusitis: Infections spreading from the sinuses to the skull base.
- Head Trauma or Surgery: Injuries that allow pathogens to enter the bone.
Pathophysiology
CSBO begins when an infection, such as chronic sinusitis, invades the
bone tissue at the base of the skull. It may spread through the sphenoid sinus, clivus, and petrous part of the temporal bone, potentially involving cranial nerves and causing neurologic deficits. This condition can be particularly dangerous because the skull base lies near critical structures like the brainstem, carotid arteries, and cranial nerves, which are vulnerable to damage from inflammation and infection.
Symptoms
CSBO often presents subtly and may mimic other neurological conditions, leading to delays in diagnosis. Key symptoms include:
- Severe headache: Often localized at the back of the head or around the face.
- Cranial nerve palsies: Involvement of the lower cranial nerves (e.g., VI, VII, IX, X, XII) can cause facial weakness, dysphagia (difficulty swallowing), or hoarseness.
- Facial pain or numbness: If the trigeminal nerve is involved.
- Hearing loss or tinnitus: In cases where the infection extends to the ear.
- Fever: Though fever may be absent in immunocompromised patients.
- Swelling and drainage from sinuses: In cases involving the sinuses.
Diagnosis
Diagnosing CSBO is challenging and often requires a combination of clinical suspicion and imaging studies.
- Imaging Studies:
- CT Scan: Useful for assessing bone erosion and sinus involvement.
- MRI with contrast: More sensitive for identifying soft tissue involvement, cranial nerve damage, and early bone marrow changes.
- Bone Scans (Technetium-99 or Gallium Scan): Helpful in identifying osteomyelitis when other imaging studies are inconclusive.
- Microbiological Studies:
- Blood cultures and sinus swabs may be performed to identify the causative organism.
- Biopsy of affected bone or sinus mucosa may be necessary, particularly if fungal infections like Aspergillus or Mucor are suspected.
- Laboratory Tests:
- Elevated C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) are common but non-specific markers of inflammation.
Management
- Medical Treatment:
- Antibiotics:
- Prolonged courses (6-12 weeks) of intravenous antibiotics targeting the suspected pathogen are required.
- Anti-pseudomonal antibiotics (e.g., piperacillin-tazobactam) are often used if bacterial infection is suspected.
- In fungal osteomyelitis, agents like voriconazole (for Aspergillus) or amphotericin B (for Mucor) are needed.
- Monitoring Treatment Response:
- Regular imaging (MRI or bone scans) helps assess the response to therapy.
- Laboratory markers like CRP and ESR should be monitored periodically.
- Antibiotics:
- Surgical Treatment:
- Surgery may be required for debridement of necrotic tissue or to drain an abscess if antibiotics alone are insufficient.
- Sinus surgery may be necessary if the infection originated from the sinuses and persists despite medical treatment.
- Hyperbaric Oxygen Therapy (HBOT): In refractory cases, HBOT may enhance bone healing and support antibiotic therapy by improving oxygenation in infected tissues.
Complications
- Cranial nerve deficits: Damage to cranial nerves can lead to facial paralysis, swallowing difficulties, and other complications.
- Intracranial extension: Infection can spread to the brain, causing meningitis or abscess formation.
- Vascular complications: Involvement of blood vessels may lead to cavernous sinus thrombosis or carotid artery rupture.
Conclusion
Central skull base osteomyelitis is a challenging condition that requires early recognition and aggressive management. A multidisciplinary approach involving infectious disease specialists, neurologists, and otolaryngologists is often necessary. Though outcomes have improved with advanced imaging, prolonged antibiotic therapy, and surgical options, patients require close follow-up to monitor for potential complications.