Introduction
Fungal infections of the ear, also known as otomycosis, occur when fungi colonize the external auditory canal. Otomycosis primarily affects the outer ear and is more common in warm, humid climates. While bacteria typically cause ear infections, fungal infections are increasingly recognized, especially among individuals with underlying risk factors such as frequent ear cleaning or moisture exposure. The most common fungi responsible for otomycosis are species of Aspergillus and Candida.
Causes and Risk Factors
Several factors predispose individuals to fungal ear infections:
- Warm, Humid Environments: Fungi thrive in moisture-rich conditions, making otomycosis more common in tropical regions.
- Frequent Swimming or Water Exposure: Known as “swimmer’s ear,” persistent water in the ear canal creates an ideal environment for fungal growth.
- Use of Ear Drops or Antibiotics: Long-term antibiotic or steroid use may alter the ear’s natural flora, encouraging fungal colonization.
- Trauma from Ear Cleaning: Excessive cleaning with cotton swabs can damage the ear canal, making it vulnerable to infection.
- Underlying Conditions: Diabetes, immunosuppression (e.g., HIV), or eczema increase susceptibility.
Symptoms of Otomycosis
Otomycosis may present with a variety of symptoms, including:
- Itching: Persistent itchiness in the ear canal is a hallmark symptom.
- Ear Discharge: White, gray, or black discharge with a musty odor may be present.
- Fullness or Blockage: Patients often experience a sensation of fullness or blockage in the ear.
- Pain: Mild to moderate pain, particularly if the infection is accompanied by swelling.
- Hearing Loss: Temporary hearing impairment may occur due to debris or fungal material blocking the canal.
Diagnosis
- Clinical Examination: A visual inspection using an otoscope may reveal fungal elements, such as fluffy white, yellow, or black spores.
- Microscopy and Culture: Samples of ear discharge can be examined to identify the specific fungus involved, such as Aspergillus niger, Aspergillus fumigatus, or Candida albicans.
- Differentiation from Bacterial Otitis Externa: Diagnosis can be complicated as symptoms overlap with bacterial ear infections, though fungal infections often involve more itching and discharge.
Treatment and Management
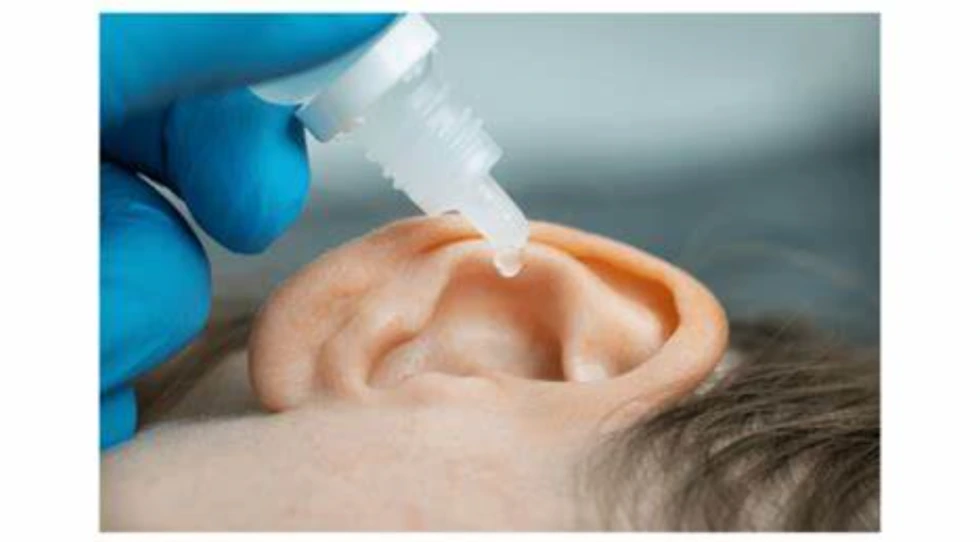
- Mechanical Cleaning
Debridement (cleaning of the ear canal) is the first step to remove fungal debris and improve the efficacy of topical medications. This is usually performed by an ENT specialist using suction or ear picks.
- Topical Antifungal Agents are the mainstay of treatment.
- Oral Antifungal Therapy
Oral antifungal medications, may be necessary in severe or recurrent infections, especially in immunocompromised individuals. - Prevention and Aftercare
– Avoid Ear Trauma: Avoid using cotton swabs or inserting objects into the ear.
– Drying the Ear: Use a towel or blow-dryer on a low setting after swimming or bathing to keep the ear canal dry.
– Prevent Recurrence: Patients in humid climates may benefit from using prophylactic acetic acid drops after water exposure.
Complications
If left untreated, otomycosis can lead to:
- Chronic Otitis Externa: Persistent infection may result in inflammation and thickening of the ear canal lining.
- Secondary Bacterial Infection: Co-infection with bacteria may occur, increasing pain and swelling.
- Spread to Middle or Inner Ear: In rare cases, the infection may spread to the middle or inner ear, particularly in immunocompromised patients.
Conclusion
Otomycosis is a common but often overlooked ear infection caused by fungal colonization of the external ear canal. While benign in most cases, the infection can be persistent and bothersome without proper treatment. Early diagnosis, mechanical cleaning, and the use of topical antifungal agents are key to successful management. Preventative measures, especially in those prone to water exposure, can reduce the risk of recurrence and improve long-term outcomes.